5 Case Studies
Case # 1
Atypical Juvenile Absence Seizures: Presentation, Diagnosis and Applications of Functional Neurology
Gilbert S. Jaudy, DC, FACFN, FABVR, CCST
Background and Aims
A 13-year-old female presented to our office complaining of seizures, fatigue due to medications and migraine headaches. The patient was with her mother and grandmother. Her mother describes that her daughter started to have extreme anxiety between the fifth and sixth grade. She could not sleep in her room alone, did not want to hang out with friends and did not go to soccer camps which she had been looking forward to attending. Her parents took her to a psychiatrist and therapist who diagnosed her with anxiety and OCD.  The doctor first put her on Zoloft but still experienced anxiety. Her grades were very poor. Prior to all these symptoms, the mother describes that her daughter had been a straight A student who was very conscious of her studies. In November of 2010 the mother describes that the daughter went into a “staring spellâ€. She was standing and staring out the glass door wall. She was not responding to her mother at all. The mother described that after about a minute she “snapped out†of it and began to describe a very vivid account of what she had just seen. The mother said that her daughter could hear her, but could not respond. The mother started to notice more of these “spellsâ€. The mother added that seizures run in her family; her sister (the mother’s) had temporal lobe epilepsy, her paternal grandmother had narcolepsy and cataplexy, and all her cousins, including herself had febrile seizures when they were younger. Immediately after, the parents took their daughter to a neurologist who ordered a sleep-deprived EEG. The EEG was 40 minutes long and documented about 8 seizures, the longest being 8 seconds. The neurologist’s report mentioned that “the patient’s EEG was consistant with three cycle per second spike and wavy activity seen mainly during the hyperventilation phase of the EEGâ€. The child was later on put on several different medications including Zarontin, Lamictal, Zoloft, Depakote, Prozac, Ethosuximide, Lunesta, Carnicor, Levocarnitine, and Vyvance, Vimpat, but seizures persisted. Several neurologists told the mother that the child’s prognosis to completely get of the seizures was very poor due to the fact that her types of seizures were changing. Medical records reveal that the child has been diagnosed by several neurologists as having atypical juvenile absence seizures coupled with anxiety, OCD (obsessive compulsive disorder), Attention Deficit Disorder, memory/disorganization problems, and static encephalopathy.  By the end of 2010, the neurologist requested an MRI of “the head with and without contrast because of the mixed absence epilepsy that was then being exhibitedâ€; which came out negative.
On 6/10/11 during consultation with Dr. Jaudy at Jaudy Treatment Center, the child described that her seizures were getting worse coupled with severe migraine headaches.
Methods
The child had undergone a comprehensive and extensive neurological examination using standard neurological tests and diagnostics including VNG and Posturography, She had sensory and motor deficiency greater on her left side. Posterior center of pressure with left deviation. She also had positive primitive reflexes and severe spastic myoclonus on the left foot,  in addition to bilateral positive Babinski and Hoffamn signs. The patient had left sided incoordination, dysmetria, left hypermetria. The patient had slow and irregular pursuits with loss of gaze.
A slow systemic Functional Neurology approach was implemented using various sensory and motor applications, coupled motion reductions, visual and auditory stimulation, cerebellar activation, complex therapeutic activities, home instructions and dietary changes.
Results
The patient responded favorably from the first visit on 6-15-11. First visit post testing revealed immediate improvement and resolution of pathological reflexes (Babinski’s and Hoffman’s). Post first treatment testing showed immediate improvement in motor and sensory function on the left side vs. the right, as well as resolution of 4 out of 5 of the primitive reflexes. By the third treatment the patient and her parents reported no seizures, staring looks, headaches or any abnormal activities. The patient was treated for 2 and a half months at an average of once a week. A complete assessment was obtained on 8-30-11 which revealed normal post neurological testing. Today the 13 -year- old lives seizure free, migraine free, and enjoys playing soccer and camping with family and friends.
Case # 2
Complex Partial Epileptic Seizures Complicated by Abnormal Clonic Movements of Extremities: A Functional Neurology Approach
Gilbert S. Jaudy, DC, FACFN, FABVR, CCST
Background and Aims
A 63 year old female presented to our clinic, accompanied by her husband, complaining of seizures since 2007, in addition to migraine headaches and high blood pressure. History of the patient consisted of allergies all her life; migraine headaches since she was 12 years old; appendectomy at age 17 and tonsillectomy at age 13. She added that in 1979 she had weakness in the legs and began falling. In 1983 she had a severe panic and hypertension attack and was taken to hospital by the paramedics. In 2007 she began having seizures, saw several neurologists and was put on several seizure medications with no change. In March of 2008, a brain MRI revealed several tiny 2-4 mm diameter foci of white matter signal alteration. On 2/22/2008 a medical neurologist ordered an EEG which showed no associated EEG rhythmic activity, however, photic stimulation induced abnormal clonic movements of all extremities. In March of 2008, a brain MRI revealed several tiny 2-4 mm diameter foci of white matter signal alteration. The patient was then diagnosed with Complex Partial Epileptic Seizures and was put on other types of medications. Her seizures kept increasing in frequency and duration which could “last all day every dayâ€. The patient fears that her seizures get worse and she will become bedridden and helpless in the next 2 years, and become a burden on her husband.
Methods
The patient had undergone a comprehensive and extensive neurological examination using standard neurological tests and diagnostics including VNG and Posturography, She had bilateral sensorimotor deficiencies, Posterior center of pressure (PCOP). She also had positive pathological reflexes. The patient had balance and incoordination issues. She also had slow saccadic movements in various planes, and loss of downward saccades. .She also had irregular pursuits, bilateral hippus with loss of gaze.
A slow systemic Functional Neurology approach was implemented using various visual, auditory, vestibular, sensory and motor applications, brain based activities, cerebellar activation, complex therapeutic activities, home instructions and dietary changes.
Results
The patient started her first visit on 2-25-10 till 3-24-10 at an average of 3 times a week. She then had to leave for a month and came back on 5-6-10 for her last visit. On 3-1-10 patients reports that she has not had any seizure activities since last treatment on 2-25-10. On 3-3-10 patient reports constant improvement without any seizure activities or migraine headaches. After then, the patient kept showing constant progress and on
3-12-10 she reported saying “I’m getting my life backâ€. Today, the patient is seizure and migraine free, and enjoys life with her husband and family.
Case # 3Â
Pseudo-complex Partial Seizures complicated by Non-Hodgkin’s Lymphoma, Stiff Man’s Syndrome, and Vertigo: Diagnosis and Applications of Functional Neurology
Gilbert S. Jaudy, DC, FACFN, FABVR, CCST
Â
Background and Aims
The patient is a 77-year-old female who presents with long-standing history of seizures, balance problems, stiffness, confusion, and loss of memory. The patient reported that she had been involved in an experimental chemotherapeutic agent for her non-Hodgkin’s lymphoma about 10 years ago, which resulted in severe vertigo and confusion. She stated that since that episode she had had issues in terms of balance and equilibrium. The patient also complains of seizures, and feels that the seizures were secondary to the chemotherapeutic agent that was initiated and administered at UCLA. She reported that she was constantly confused, fell 5-6 times a day, seizure tremors, great difficulty speaking, dropping things and stuttering  “after use of experimental drug while taking chemo†in 2002. She also has a history of DJD, low back pain, neck pain, muscle spasms, leg cramps, jaw pain, painful joints, migraines, fatigue and fainting.
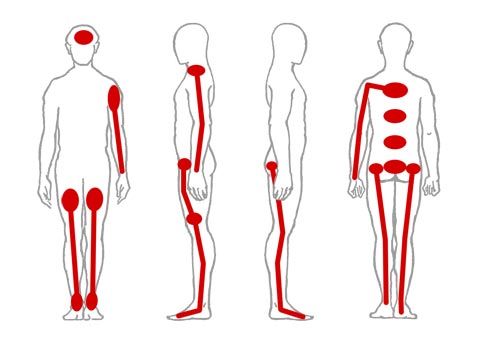
The illustration below shows the areas of pain that the patient marked on the history intake form.
 A multidetector CT of the brain without intravenous contrast obtained in 2006 revealed punctate calcification within the right lenticular basal ganglion nucleus.
A bilateral carotid ultrasound examination obtained in 2006, revealed mild atheromatous plaque formation in the distal common carotid artery, bulbar area and proximal internal carotid artery on the left side without significant stenosis. Minor atheromatous changes in the proximal right internal carotid artery.
The patient was put on several seizure and pain medications, and was administered IVIG infusions for the lymphoma.
On 04/08/2011 a brain MRI showed accelerated patchy periventricular and centrum semiovale microangiopathic signal changes with mild atrophy.
Â
Methods
A comprehensive and extensive neurological examination was performed, using standard neurological tests and diagnostics including VNG and Posturography, Tremorscope, and Physilogical Blind spot Mapping. She had bilateral sensorimotor deficiencies, in addition to incoordination, dysmetria, disequilibrium, dyskinesia, abnormal gait, severely irregular pursuits, absent VOR, intention tremors, hyperreflexia, carotid bruits, and allodynia..
A systemic caudal to rostral Functional Neurology approach, addressing central nervous system, peripheral nervous system, autonomic nervous system, and skeletal musculature,  was implemented using various sensory and motor applications, visual and auditory stimulation, cerebellar activation, complex therapeutic activities, home instructions and dietary changes.
Brain-Based Activities were instructed targeting mesencephalic-dentato-rubro-thalamo-cortical pathways.  Oxygen therapy was administered. Unilateral nasal breathing  excercises and anti-inflammatory nutraceuticals.
Results
Functional Neurology addresses different faulty pathways which lead to brain plasticity, remapping and proto oncogene in the nucleotide sequence. It’s been diagnostically determined that through specific and gradual applications in Functional Neurology the patient’s seizure disorder, migraines, imbalance, and tremors were contained. Today, the patient today is seizure free, and symptom free. She enjoys a normal life with her husband, something she has not been able to realize for over 30 years.
Case # 4
The Impact of Neuro-Visceral Applications and Brain Re-mapping on Hashimoto’s: A Functional Neurology Approach.
Gilbert S. Jaudy, DC, FACFN, FABVR, CCST
Background and Aims
The patient is 53-year-old female who presented to our clinic on 8/25/08 complaining of thyroid issues, knee pain, general body pain, and back pain. The patient reported that she was diagnosed with Hashimoto’s disease by her family doctor who is deceased. The patient reported that her pain was a 10/10, on a scale of 1 to 10, 10 being the worst. Sha has had a past medical history of fractured bones, high blood pressure, balance problems, eye pain, blurred vision, belching and gas, gallbladder problems (cholecystectomy), jaw pain, stiffness, chest apin, headaches, dizziness, tremors, hemorrhoids, back/neck pain, shoulder/arm pain, knee/ankle pain, painful joints, weight gain, swollen joints, leg cramps, hip/leg pain, and fatigue. The patient has had three c-sections, bilateral carpal tunnel surgeries, cholecystectomy, and left lobe thyroidectomy. The patient was put on several thyroid medications including levothyroid, levoxyl, and synthroid. She reported an overall feeling of ill-being and increase in her symptoms as well as difficulty walking.
Methods
The patient had undergone a comprehensive and extensive neurological and physical examination using standard neurological tests and diagnostics including VNG,  posturography, tremorscope, blind spot mapping, She had global sensory and motor deficiencies, in addition to incoordination, cerebellar dysmetria, hyperreflexia, allodynia, anisocoria, posterior center of pressure, asterixis, dyskinesia, frontal release signs, ocular dysmetria, loss of  upward and downward saccades compared to horizontal ones.
Systemic Functional Neurology procedures and applications were implemented using various sensory and motor applications, coupled motion reductions, visual and auditory stimulation, cerebellar activation, complex therapeutic activities, home instructions, timed breathing excercises, oxygen therapy and various specific mitochondrial neutraceuticals and phytonutrients. Various applications were administered at an average of 3 times a week for 2 weeks. Then, once a week for 4 weeks.
Results
Within 12 visits the patient’s Hashimoto’s symptoms were stabilized. A thyroid antibodies lab test for TPO’s and antithyroglobulin was ordered on 1-5-2011, which came negative. Today the patient’s symptoms have decreased by 90 % and is currently able to do all her daily activities with hardly any complaints.
Â
Case # 5
Procedures and Applications of Functional Neurology in the Treatment Hearing Impairment / Deafnesss
Gilbert S. Jaudy, DC, FACFN, FABVR, CCST
Background and Aims
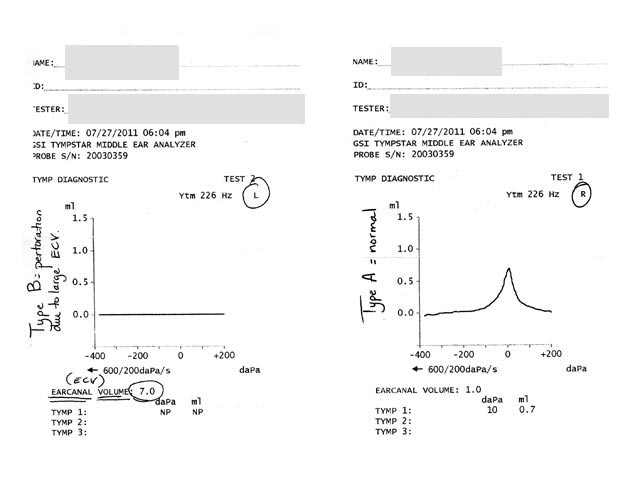
The patient is a 15-year-old who presented to our clinic complaining of hearing impairement. Her parents reported that they started noticing their daughter’s hearing problems since the age 3 to 4 years. They also reported that her hearing got progressively worse over the years, which affected her ability to learn, socialize and even speech fluency. Her parents reported that for many years she has lost interest to make friends and felt secluded. She always had difficulty hearing in class, and felt very embarrassed in front of her friends and teachers. Her hearing impairment affected her grades and schooling activities. The mother reports that her daughter would have to be very close to the sound source, which had to be very high, and if it was a person then she would have to look at the lips with high sound to be able to pick up few words. Her mother reports that at the age of 7 year old, she had bilateral ear tubes put in to drain the fluid out of the ear.  However, her hearing impairement started way before the ear tubes. A audiology examination revealed an ECV of 7.0 in the left ear Further otoscopic evaluation  showed a hole in the left ear drum. The patient hearing deficiency progressively got worse.
Â
A tympanogram showing an ECV of 7.0 in the left ear, 2 weeks pre-treatment
 Methods
Comprehensive neurological examination was performed including an otoscopic and vestibular examination. Weber’s test revealed sound hardly heard in the right ear.   A vestibular examination revealed left anterior, and right posterior ear canal angulation in the right yaw plane coupled with a posterior center of pressure, and right ellipse. The patient’s primitive reflexes (startle reflex, ATNR, spinal gallant) were positive bilaterally with more exacerbation on the left. She had right muscle paresis and left disdiadochokinesis. Dual tasking revealed a slow-freezing gait, and decreased ability to follow instructions. Palpation of paraspinal musculature revealed spacticity on left suboccipital musculature, and right anterior SCM/pectoralis muscles.
Cerebellar activation excercises were administered on the left side coupled by timed breathing excercises, metronome timed activities, oxygen therapy and various specific physical excersices coupled with right yaw eye movement. The patient was treated for 2 weeks on daily basis.
Results
Patient hearing was 90 % restored, in addition to resolution of her primitive reflexes, and other neurological deficiencies.
Â
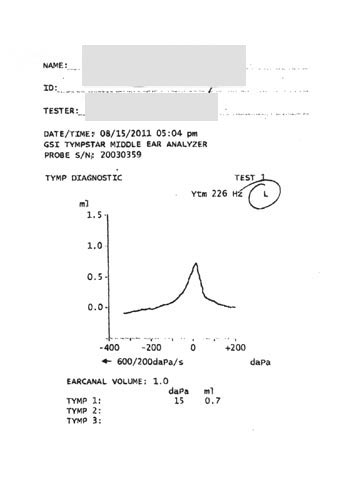
A tympanogram obtained 2 weeks post treatment revealed normal ECV.
*All presentations are clinically documented.